Understanding Actinomycosis: Symptoms, Causes & Treatment | Discover
Is that persistent swelling on your jawline something to be concerned about? Actinomycosis, a relatively rare but serious bacterial infection, might be the hidden culprit, and it's time to understand this often-misdiagnosed condition.
The microscopic world often holds surprises, and sometimes, those surprises manifest as unwelcome guests in our bodies. One such guest is Actinomyces israelii, the bacterium primarily responsible for causing actinomycosis. This bacterium, normally a benign resident of our upper respiratory tract, mouth, and digestive system, can transform into a formidable foe under the right circumstances. While often overlooked or misdiagnosed, understanding the intricacies of actinomycosis is vital for timely intervention and effective treatment.
Actinomycosis, despite its infrequency, presents a significant clinical challenge. Its insidious nature and varied presentations, often mimicking other, more common infections, make early diagnosis a hurdle. Furthermore, the disease's ability to spread and cause significant tissue damage necessitates a comprehensive approach to management. From the initial diagnostic suspicion to the prolonged treatment regimens, the journey through actinomycosis requires the expertise of medical professionals and the resilience of the patient. This article will delve into the complexities of actinomycosis, providing a clear understanding of its causes, symptoms, diagnostic approaches, and treatment strategies. Our goal is to shed light on this obscure infection and equip both patients and healthcare providers with the necessary knowledge to combat this challenging disease effectively.
The origins of actinomycosis lie in the soil and within the human body. The Actinomyces species, particularly Actinomyces israelii, are gram-positive, anaerobic or microaerophilic bacteria. These bacteria thrive in environments devoid of oxygen or with very low oxygen levels. Normally, they coexist peacefully in the oral cavity, the gastrointestinal tract, and the female genital tract. However, when the normal mucosal barriers are breached due to trauma, surgery, or underlying conditions, these bacteria can invade deeper tissues, initiating the infection. The bacteria's ability to cause infection hinges on its unique characteristics, including its capacity to form a complex inflammatory response, characterized by the formation of abscesses and draining sinuses. The infection is typically slow-progressing, often developing over weeks or months, complicating early recognition and diagnosis. The varied clinical presentations and the involvement of multiple body sites further complicate the diagnostic process.
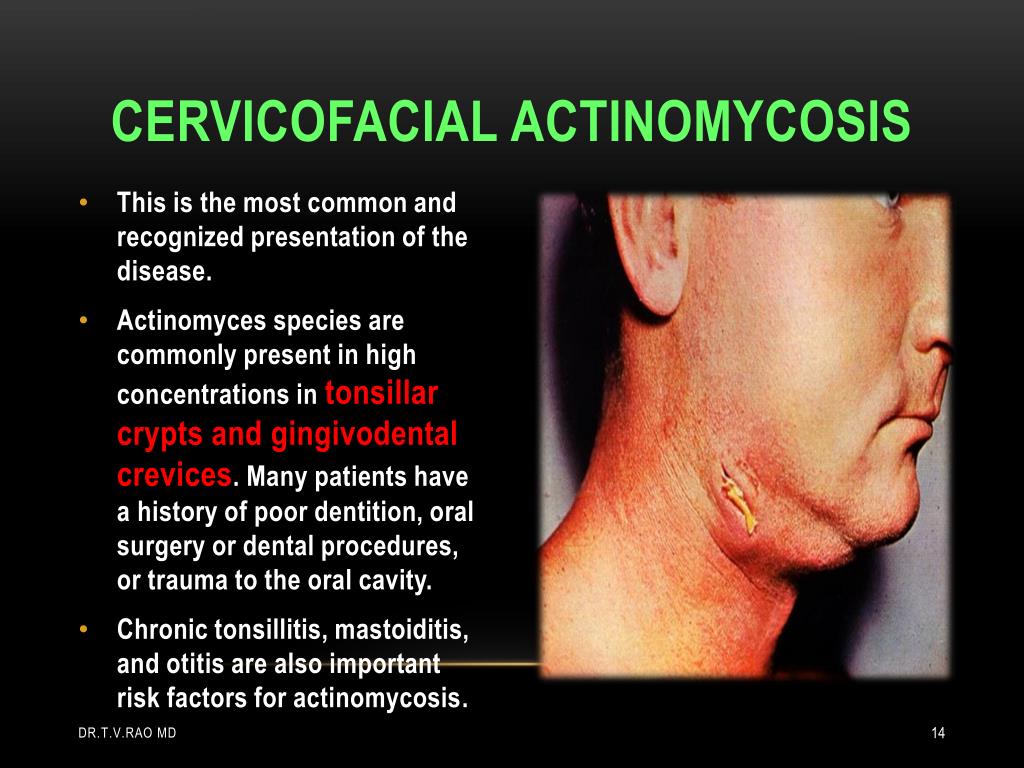
Actinomycosis manifests in several forms, varying with the affected body area. Cervicofacial actinomycosis is the most frequently observed form, accounting for approximately 50% of all cases. This form often originates from dental procedures, oral injuries, or poor oral hygiene, providing the bacterium with an entry point. In this manifestation, the infection typically presents as a slowly progressing, indurated swelling in the jaw or neck area. The swelling is usually painless in the early stages, but as the infection advances, pain, trismus (difficulty opening the mouth), and the formation of abscesses become more pronounced. Over time, the abscesses can rupture, forming draining sinuses that discharge pus, often containing characteristic "sulfur granules," which are clumps of bacteria.
Pulmonary actinomycosis is another important presentation, which arises when the bacteria are inhaled or aspirated into the lungs. This form can mimic pneumonia or lung abscesses, causing symptoms such as cough, chest pain, fever, and hemoptysis (coughing up blood). The progression can be slow and insidious, leading to delays in diagnosis. The diagnostic challenge is further compounded by the difficulty in differentiating it from other pulmonary infections. The involvement of the lungs poses significant risk, and early intervention is crucial to prevent complications, including empyema (pus in the pleural space) and spread of the infection.
Abdominal actinomycosis is a less common but severe form, typically resulting from disruptions of the gastrointestinal tract or abdominal surgeries. This can lead to the formation of abdominal abscesses, peritonitis (inflammation of the abdominal lining), and the involvement of surrounding organs. The symptoms may include abdominal pain, fever, and changes in bowel habits. The diagnosis in this location can be exceptionally challenging, and it often necessitates imaging studies and sometimes surgical exploration to rule out other conditions like cancer or other infections. Pelvic actinomycosis, particularly in women using intrauterine devices (IUDs), is also possible, potentially leading to pelvic abscesses and related complications.
Because of the bacteria's normal location in the nose and throat, actinomycosis most commonly affects the face and neck, a condition that can also arise following oral injuries or dental work, which opens the door for the bacteria to invade tissue. As the infection develops, it creates characteristic swellings and abscesses, often accompanied by draining sinuses. These sinuses, a telltale sign of actinomycosis, release pus that sometimes contains distinctive sulfur granulessmall, yellowish clumps of bacteria. The presence of these granules, coupled with the infection's chronic nature and slow progression, is crucial in distinguishing actinomycosis from other infections that may show similar symptoms.
Actinomycosis can also be found in the lungs. Pulmonary actinomycosis mirrors conditions like pneumonia or lung abscesses. Patients often experience coughs, chest pain, fever, and occasionally cough up blood. The slow-paced progression of this form can complicate timely diagnosis, making it crucial to consider actinomycosis when typical treatments for lung infections prove ineffective. Diagnosing this form often involves a combination of imaging techniques, such as chest X-rays or CT scans, and lab tests to identify the bacteria accurately.
Moreover, actinomycosis can affect the abdomen and pelvis, often occurring after abdominal surgeries or due to trauma in the abdominal region. This can lead to abdominal abscesses, peritonitis (inflammation of the abdominal lining), and involvement of neighboring organs. Pelvic actinomycosis is sometimes seen in women using intrauterine devices (IUDs). The symptoms include abdominal pain, fever, and changes in bowel habits, thus adding to the complexity of diagnosis.
The diagnosis of actinomycosis can be complex, requiring a combination of clinical assessment, imaging techniques, and microbiological investigations. The initial step typically involves a detailed medical history and physical examination, focusing on the location of the symptoms and any potential risk factors. Imaging modalities, such as X-rays, CT scans, and MRIs, are crucial in identifying abscesses and assessing the extent of tissue involvement. These imaging studies help to define the size and the boundaries of the infected area, assisting in the planning of treatment.
Microbiological confirmation is essential for a definitive diagnosis. This typically involves culturing the bacteria from the pus drained from an abscess or a tissue sample obtained through biopsy or surgical procedures. The Actinomyces bacteria are fastidious, meaning they require special growth conditions, including anaerobic or microaerophilic environments, for proper growth in the laboratory. The identification of the bacteria may take several days or even weeks. The classic finding of "sulfur granules" in the pus is highly suggestive of actinomycosis but should be confirmed by microbiological analysis.
Treatment for actinomycosis usually involves a combination of antimicrobial therapy and, in many cases, surgical intervention. The cornerstone of treatment is the use of antibiotics, particularly high doses of penicillin, as Actinomyces species are generally susceptible to this antibiotic. Other antibiotics, such as tetracycline, erythromycin, clindamycin, and doxycycline, may be considered, particularly in patients who are allergic to penicillin. The duration of antibiotic therapy is typically prolonged, often lasting several weeks to months, to ensure complete eradication of the infection. The extended duration helps to prevent recurrence. Intravenous antibiotics may be necessary in severe cases or when oral medication absorption is compromised, and the switch to oral antibiotics can be made once the patient shows clinical improvement.
Surgical intervention plays a critical role in the management of actinomycosis, especially in cases with large abscesses or when there is extensive tissue involvement. Surgical procedures may include incision and drainage of abscesses, debridement of infected tissue, and the removal of fistulous tracts. Surgical intervention, in conjunction with antibiotic therapy, helps to control the infection, promote healing, and prevent complications. In some cases, surgical intervention can provide tissue samples for diagnosis and assist with antibiotic penetration to the site of infection.
Prognosis in actinomycosis is generally good with early diagnosis and prompt treatment. The cure rate is high, particularly when a combination of antibiotics and surgical intervention is employed. The outcome depends on factors such as the extent of the infection, the location of the infection, the immune status of the patient, and the timeliness of diagnosis and treatment. Complications such as spread of the infection to other organs, the development of chronic fistulas, and treatment failure are more likely in patients with delayed diagnosis, underlying medical conditions, or inadequate therapy. Patients with weakened immune systems may also be at higher risk of adverse outcomes.
The prevention of actinomycosis is primarily based on good oral hygiene and prompt treatment of any oral injuries or infections. Regular dental check-ups, proper brushing, and flossing can help to prevent the spread of Actinomyces species. Early detection and treatment of oral infections and injuries will help to prevent the spread of the bacteria. Patients with compromised immune systems, those undergoing procedures involving the oral cavity, or those with chronic conditions should receive special attention to prevent the development of this opportunistic infection. In addition, providing education about the signs and symptoms of actinomycosis can facilitate early recognition and prompt medical intervention.
In summary, actinomycosis is a rare but significant bacterial infection that requires a high index of suspicion for diagnosis. Understanding the epidemiology, clinical presentations, and diagnostic approaches is essential. The effectiveness of the treatment depends on a combination of antimicrobial therapy and surgical intervention. With early diagnosis, proper treatment, and follow-up, patients can achieve a good outcome and successfully overcome this challenging infectious disease. Further research is needed to improve diagnostic methods, optimize treatment strategies, and understand the mechanisms that contribute to the pathogenesis of actinomycosis.
| Aspect | Details |
|---|---|
| Name | Actinomycosis |
| Type | Infectious Disease |
| Causative Agent | Actinomyces bacteria (primarily Actinomyces israelii) |
| Common Locations | Face, neck (cervicofacial actinomycosis), lungs (pulmonary actinomycosis), abdomen (abdominal actinomycosis), pelvis (pelvic actinomycosis) |
| Symptoms |
|
| Diagnosis | Clinical assessment, imaging (X-rays, CT scans, MRIs), microbiological cultures |
| Treatment | Prolonged antimicrobial therapy (e.g., penicillin), surgical intervention (incision, drainage, debridement) |
| Prognosis | Generally good with early diagnosis and appropriate treatment |
| Risk Factors | Dental procedures, oral injuries, poor oral hygiene, aspiration, abdominal trauma, use of IUDs |
| Reference | National Center for Biotechnology Information (NCBI) |
It is crucial to consult with healthcare professionals for proper diagnosis and treatment. Self-treating can lead to complications and worsening of the condition.