Hodgkin Vs. Non-Hodgkin Lymphoma: Which Is Easier To Treat?
Is one form of lymphoma inherently "better" than the other in terms of treatment success? The reality is complex, but generally speaking, Hodgkin lymphoma boasts a higher cure rate than Non-Hodgkin lymphoma, particularly in its earlier stages, thanks to advancements in therapies over the past few decades. This isn't to diminish the challenges faced by those battling Non-Hodgkin lymphoma; the landscape of treatment is constantly evolving, and outcomes are improving across the board. The key lies in understanding the nuances of each disease, their respective subtypes, and the factors that influence a patient's response to treatment.
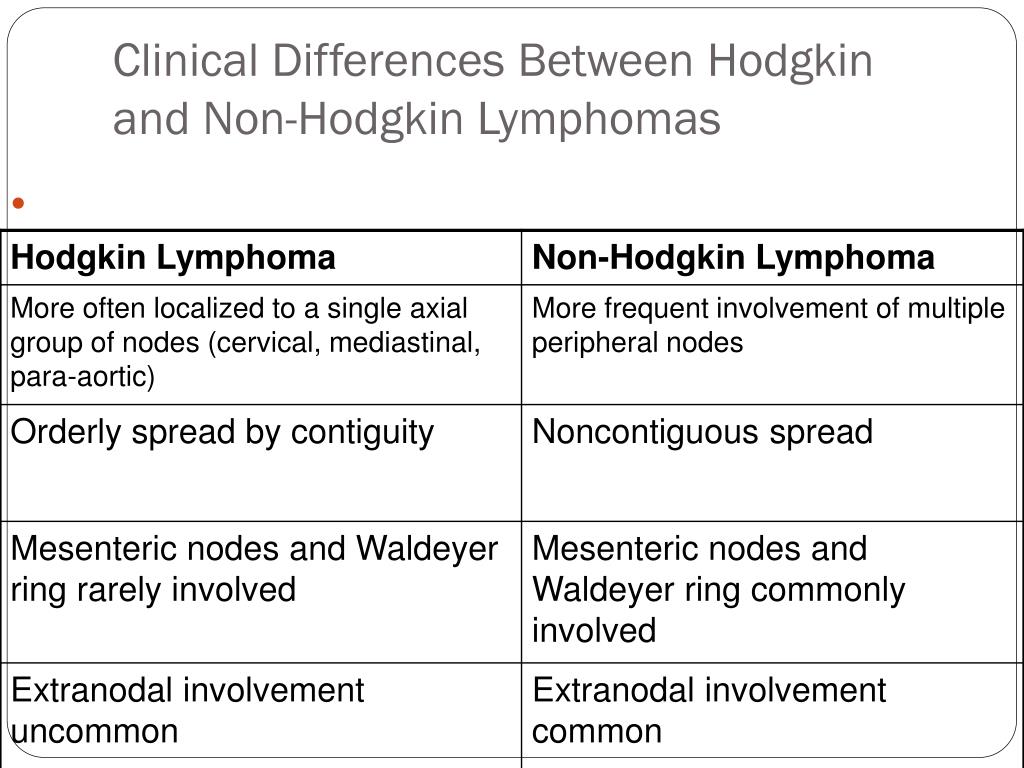
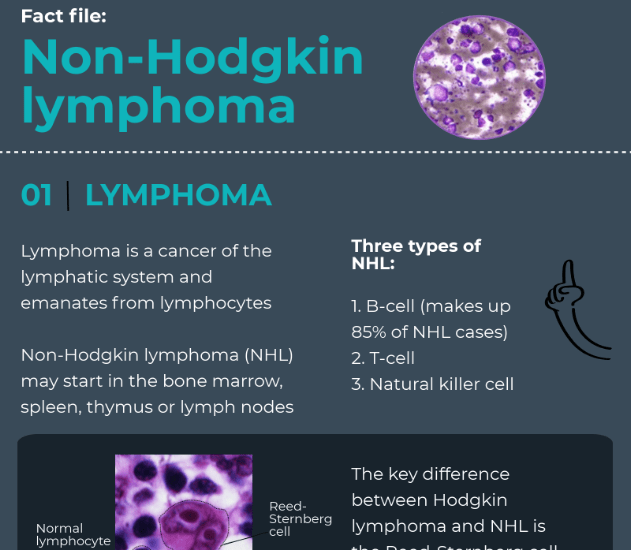
When faced with a diagnosis of lymphoma, a natural question is often, "Which type am I dealing with, and what are my chances?" Both Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL) are cancers that originate in the lymphatic system, a crucial part of the immune system. The lymphatic system comprises a network of vessels, lymph nodes, and organs that help fight off infections and diseases. Lymphoma arises when lymphocytes, a type of white blood cell, begin to grow and divide uncontrollably. However, the two types differ fundamentally in their cellular origin and behavior. The presence of a specific type of abnormal cell, the Reed-Sternberg cell, is the defining characteristic of Hodgkin lymphoma. Its absence is the defining factor for Non-Hodgkin lymphoma, a more diverse group encompassing over 90 different subtypes, each with its own characteristics, treatment approaches, and prognoses. This heterogeneity is why broad generalizations about treatability can be misleading. A more accurate assessment requires a precise diagnosis of the specific subtype and a careful evaluation of the individual patient's condition.
| Attribute | Details |
|---|---|
| Name of Condition | Hodgkin Lymphoma vs. Non-Hodgkin Lymphoma (Treatability Comparison) |
| Overview | A comparison of two major types of lymphoma, focusing on their relative treatability, prognosis, and treatment approaches. |
| Defining Feature (Hodgkin Lymphoma) | Presence of Reed-Sternberg cells. |
| Defining Feature (Non-Hodgkin Lymphoma) | Absence of Reed-Sternberg cells; a highly diverse group encompassing numerous subtypes. |
| Key Consideration | Stage of diagnosis, subtype of NHL, and individual patient factors significantly influence treatment success. |
| Treatment Approaches (General) | Chemotherapy, radiation therapy, targeted therapy, immunotherapy, and stem cell transplantation. |
| Prognosis (General) | HL often has a higher cure rate, especially in early stages; NHL outcomes vary widely based on subtype and stage. |
| Importance of Subtype Identification | Critical for determining the most effective treatment strategy and predicting the patient's response. |
| Recent Advancements | Improved chemotherapy regimens, targeted therapies, and immunotherapies have improved outcomes for both HL and NHL. |
| Reference | American Cancer Society - Treating Hodgkin Lymphoma |
The distinction between Hodgkin lymphoma and Non-Hodgkin lymphoma is not just a matter of nomenclature; it's a critical factor in determining the course of treatment and the likelihood of a successful outcome. Hodgkin lymphoma, characterized by the presence of Reed-Sternberg cells, is generally considered to be the more treatable of the two, particularly when diagnosed in its early stages. This is due, in part, to the responsiveness of Hodgkin lymphoma to traditional therapies like chemotherapy and radiation. Furthermore, significant advances in chemotherapy regimens have greatly improved survival rates for Hodgkin lymphoma patients over the years. Early detection is paramount; when diagnosed and treated promptly, many patients with Hodgkin lymphoma can achieve long-term remission and even be considered cured.
Non-Hodgkin lymphoma, on the other hand, presents a more complex challenge. With over 90 different subtypes, the disease's behavior and response to treatment can vary significantly. Some subtypes, such as diffuse large B-cell lymphoma (DLBCL), are aggressive but often curable with intensive chemotherapy and other therapies. Others, such as indolent lymphomas, may progress slowly and require less aggressive treatment initially, though they can become more aggressive over time. The heterogeneity of NHL underscores the importance of accurate diagnosis and the tailoring of treatment to the specific subtype. The International Prognostic Index (IPI) is a frequently used tool to help assess the prognosis in aggressive Non-Hodgkin Lymphomas and guide treatment decisions, considering factors such as age, stage, performance status, and other characteristics.
Staging is crucial in both HL and NHL, using the Ann Arbor Staging system to determine the extent of the disease's spread. This information is vital for treatment planning, as the stage of the cancer influences the choice of therapies and the expected prognosis. Early-stage disease often involves localized treatment, such as radiation therapy or a shorter course of chemotherapy. Advanced-stage disease, where the cancer has spread to multiple lymph nodes or other organs, typically requires more intensive systemic treatment, often a combination of chemotherapy and, in some cases, stem cell transplantation. Newer therapies, such as targeted therapies and immunotherapies, are also playing an increasingly important role, particularly in the treatment of relapsed or refractory disease.
Chemotherapy remains a cornerstone of treatment for both HL and NHL. The specific drugs used and the duration of treatment depend on the subtype of lymphoma, the stage of the disease, and the patient's overall health. For Hodgkin lymphoma, a common regimen involves a combination of drugs, often including bleomycin, vinblastine, doxorubicin (Adriamycin), and dacarbazine (ABVD). For Non-Hodgkin lymphoma, treatment regimens vary widely depending on the subtype, but common drugs include cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The side effects of chemotherapy can be significant, including nausea, fatigue, hair loss, and increased susceptibility to infections. Supportive care, such as anti-nausea medications, blood transfusions, and antibiotics, plays a critical role in helping patients manage these side effects and complete their treatment.
Radiation therapy is also a vital tool, particularly for localized disease. It involves using high-energy rays to kill cancer cells. Radiation therapy may be used alone or in combination with chemotherapy, depending on the type and stage of lymphoma. It's often used to treat areas where the lymphoma is most concentrated, such as lymph nodes or organs affected by the disease. While effective, radiation therapy can also cause side effects, such as skin changes, fatigue, and damage to surrounding healthy tissues. The benefits of radiation therapy are carefully weighed against the potential risks to optimize treatment outcomes.
Targeted therapies represent a major advancement in the treatment of both HL and NHL. These drugs are designed to target specific molecules or pathways that are involved in the growth and spread of cancer cells. For example, rituximab, a monoclonal antibody, targets the CD20 protein found on the surface of B-cells and is commonly used to treat B-cell lymphomas. Other targeted therapies include Bruton's tyrosine kinase (BTK) inhibitors, such as ibrutinib, and phosphoinositide 3-kinase (PI3K) inhibitors. These drugs offer a more precise approach, potentially reducing side effects compared to traditional chemotherapy. Targeted therapies are often used in combination with chemotherapy or as maintenance therapy to prevent recurrence.
Immunotherapy is another promising approach. It harnesses the power of the patient's immune system to fight cancer. Checkpoint inhibitors, such as pembrolizumab and nivolumab, are a type of immunotherapy that blocks proteins that prevent T-cells from attacking cancer cells. These drugs are increasingly being used in the treatment of Hodgkin lymphoma and are showing promising results in some subtypes of Non-Hodgkin lymphoma. Another form of immunotherapy, CAR-T cell therapy, involves modifying a patient's own T-cells to recognize and attack cancer cells. CAR-T cell therapy has shown remarkable success in treating certain types of aggressive lymphomas, especially when other treatments have failed, and is a rapidly evolving field.
Stem cell transplantation, also known as bone marrow transplantation, is sometimes used to treat both Hodgkin lymphoma and Non-Hodgkin lymphoma, particularly in cases of relapsed or refractory disease. There are two main types: autologous stem cell transplantation, where the patient's own stem cells are collected and then returned after high-dose chemotherapy; and allogeneic stem cell transplantation, where stem cells are donated by a matched donor. Stem cell transplantation is a complex procedure with significant risks, but it can be a life-saving option for some patients. It is often used after high-dose chemotherapy to restore the blood-forming cells and enable the body to recover from intensive treatment.
The treatment landscape for lymphoma is constantly evolving. Researchers are continually investigating new therapies and treatment approaches. Clinical trials play a crucial role in advancing the field, allowing patients access to novel treatments that may not yet be widely available. Patients diagnosed with lymphoma are encouraged to discuss clinical trial options with their doctors. The participation in clinical trials contributes not only to the patient's potential benefit but also to advancements that benefit future patients.
The prognosis for both Hodgkin lymphoma and Non-Hodgkin lymphoma is influenced by a multitude of factors. For Hodgkin lymphoma, the stage of the disease at diagnosis is a significant predictor of outcome. Early-stage disease has a high chance of being cured, while advanced-stage disease may require more intensive treatment. Other factors, such as the presence of certain symptoms, the response to initial treatment, and the presence of bulky disease, can also affect the prognosis. For Non-Hodgkin lymphoma, the prognosis is highly dependent on the subtype. Some subtypes are slow-growing and may have a good long-term outcome, while others are aggressive and require prompt and intensive treatment. The International Prognostic Index (IPI) is frequently used to assess prognosis in aggressive NHL, considering factors such as age, stage, performance status, and other clinical features.
The quality of life for lymphoma patients is a critical consideration. Treatment can be physically and emotionally challenging. Managing side effects, maintaining a healthy lifestyle, and seeking psychosocial support are important aspects of care. Support groups, counseling, and resources from organizations like the Leukemia & Lymphoma Society (LLS) provide valuable assistance to patients and their families. Survivorship care is becoming an increasingly important focus, addressing the long-term effects of treatment and promoting overall well-being. Regular follow-up appointments, monitoring for potential late effects of treatment, and lifestyle recommendations contribute to a better quality of life for lymphoma survivors.
In conclusion, while the question of which is "more treatable" between Hodgkin and Non-Hodgkin lymphoma often arises, it is not a simple one. Hodgkin lymphoma often has a better prognosis, particularly in its early stages, due to its responsiveness to conventional treatments. However, the diverse nature of Non-Hodgkin lymphoma makes it essential to focus on the specific subtype, stage, and individual patient characteristics to determine the best treatment approach and predict the likely outcome. The advancements in targeted therapies, immunotherapies, and supportive care, along with continued research, are leading to improved outcomes and better quality of life for all lymphoma patients.